Do All Insurance Companies Cover Covid Testing
Shots - Health News Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show. COVID-19 testing would continue to be covered with no cost-sharing by private and public insurers for all tests consumers independently seek.
Travel Documents And Entry Requirements Prepare For Your Trip
Government also pre-paid for COVID-19 vaccines.
Do all insurance companies cover covid testing. Centene will cover COVID-19 testing and screening services for Medicaid Medicare and Marketplace members and is waiving all associated member cost share amounts for COVID-19 testing and screening. Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive. The company will not require prior authorization prior certification prior notification or step therapy protocols for these services.
There are many factors that can affect coverage and its up to you to sort them out. In March 2020 then-President Donald Trump signed the Coronavirus Aid Relief and Economic Security Act which required health insurance companies to cover COVID-19 testing and vaccinations at no. The wide variation in prices for such a simple test from 20 to over 1400 is shocking.
In doing so they required the vaccine to be available at no cost to anyone insured or not. Federal law requires all private insurance plans to cover the entire cost of COVID-19 testing. There are 2 types of COVID-19 tests.
The court found that the majority of nine business interruption BI policies put before it for scrutiny would not need to be paid out by. While a COVID-19 test should be covered under the CARES Act there are other charges that some facilities or providers can tack on that will not be covered meaning youll get stuck with a bill. Beneficiaries of a person who dies after getting the vaccine cannot collect life insurance payments.
And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test. Testing for COVID-19 is important to slowing the spread of COVID-19. So long as the test is deemed medically appropriate a November 2020 KFF analysis reportedt.
Through May 31 all BCBS companies including the BCBS Federal Employee Program FEPare. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. US insurance companies will cover costs of COVID-19 testing and treatment Companies said there would not be surprise billing for treatment.
The Medicare price for a Covid Test is 35-50. Insurance companies overwhelmingly win crucial test case on COVID payments. Covid-19 Diagnostic Testing Prices.
Although COVID-19 testing is becoming more readily available some health care insurers arent quick to cover the cost of precautionary testing. We encourage you and your health care provider to use FDA-authorized tests. Diagnostic tests determine if you are currently infected with COVID-19.
On top of that there may also be costs associated with the office or clinic visit. All private insurance has to cover 100 of the cost of COVID-19 testing Pollitz said she is miffed that employers are trying to argue otherwise. United Healthcare and Blue Cross Blue Shield of Kansas City Mississippi and South Carolina will cover costs for testing if ordered by a health care provider or physician Axios reported Wednesday.
The Federal Court ruling on a crucial test case means that insurance companies may potentially avoid paying out billions in payouts. All comprehensive health insurance companies must cover 100 of coronavirus testing and treatment according to the Federal stimulus package known as the Coronavirus Aid Relief and Economic. The Families First Coronavirus Response Act and CARES Act do not require an insurance company to pay for a test unless you have symptoms or a known or recent exposure to COVID-19 and it has been determined to be medically necessary for you by an attending healthcare provider.
Insurance companies are only required to pay for a COVID test if the individual is symptomatic or has a known or recent exposure to COVID and the test is determined to be medically necessary by a. It Depends. Chart by author.
Waiving cost-sharing for COVID-19 testing and treatment. Medicare reimburses up to 100 for the COVID test.
Covid Insurance For Foreigners In Thailand
Testing For Covid 19 Faqs Blue Shield Of Ca
Covid 19 Testing Campus Health Services
If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr
National Health Insurance Administration Ministry Of Health And Welfare Taiwan Can Help National Health Insurance S Contribution In Combating Covid 19
Test Trace Corps Testing Nyc Health Hospitals
Private Health Coverage Of Covid 19 Key Facts And Issues Kff
Covid 19 Testing Tufts Medical Center
Iso International Student Insurance
How Americans Can Get A Covid Test In Mexico The Washington Post
Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker
If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr
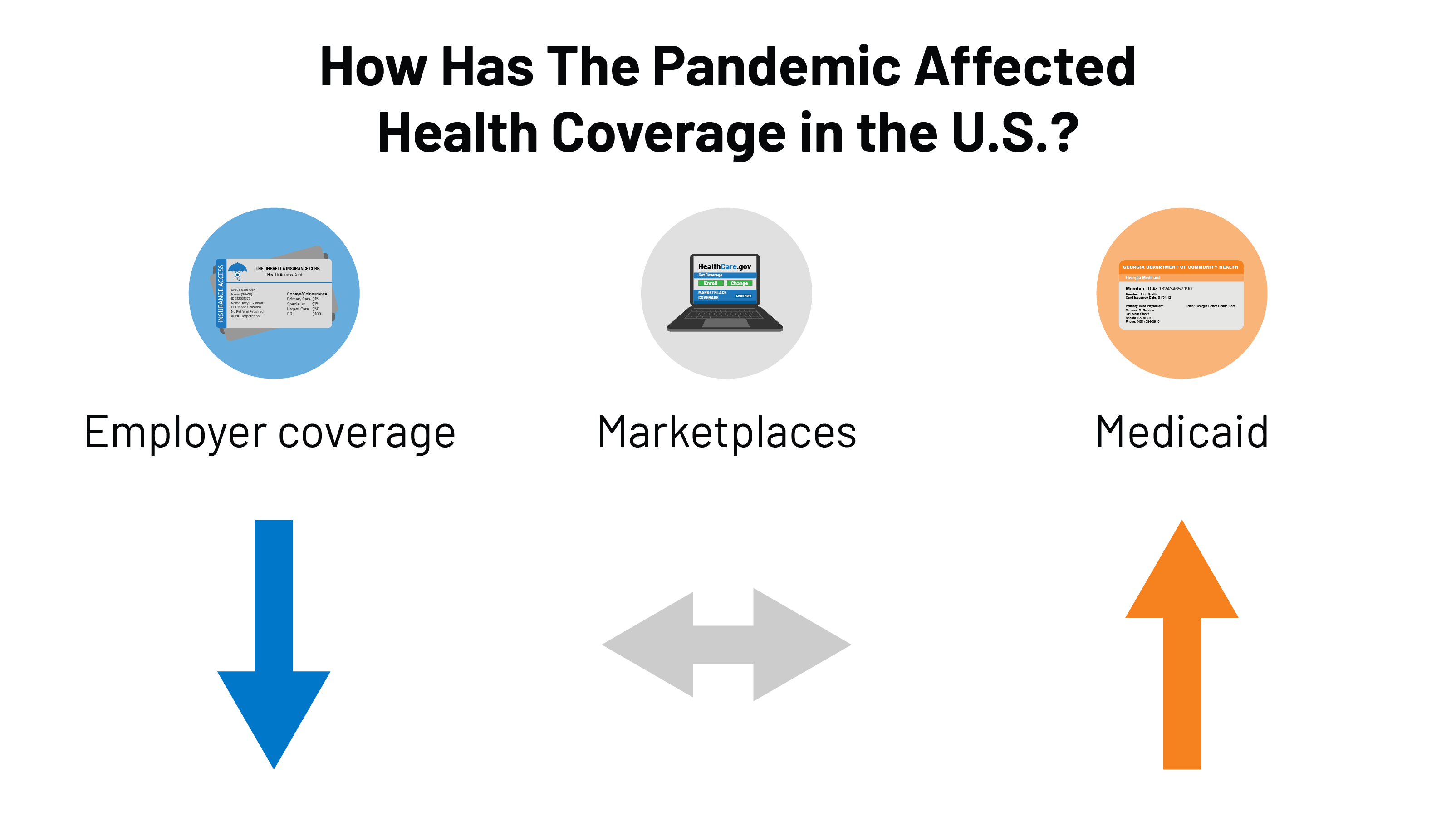
How Has The Pandemic Affected Health Coverage In The U S Kff
If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr
Limitations Of The Program For Uninsured Covid 19 Patients Raise Concerns Kff
State Covid 19 Data And Policy Actions Kff




Posting Komentar untuk "Do All Insurance Companies Cover Covid Testing"