Does Blue Cross Fep Cover Covid Antibody Test
These are covered based on your benefit plan. A doctor must order a COVID-19 test for you.
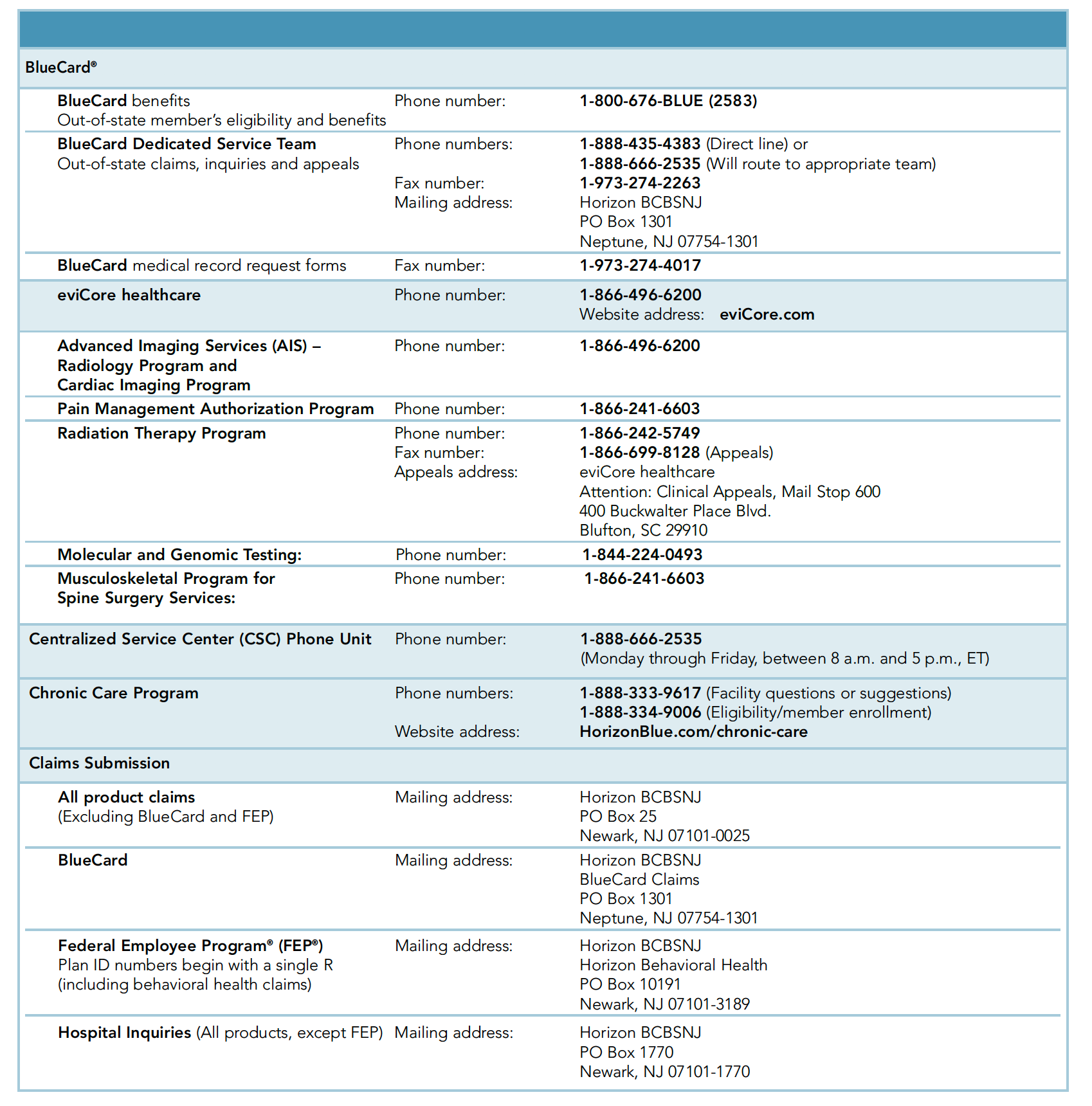
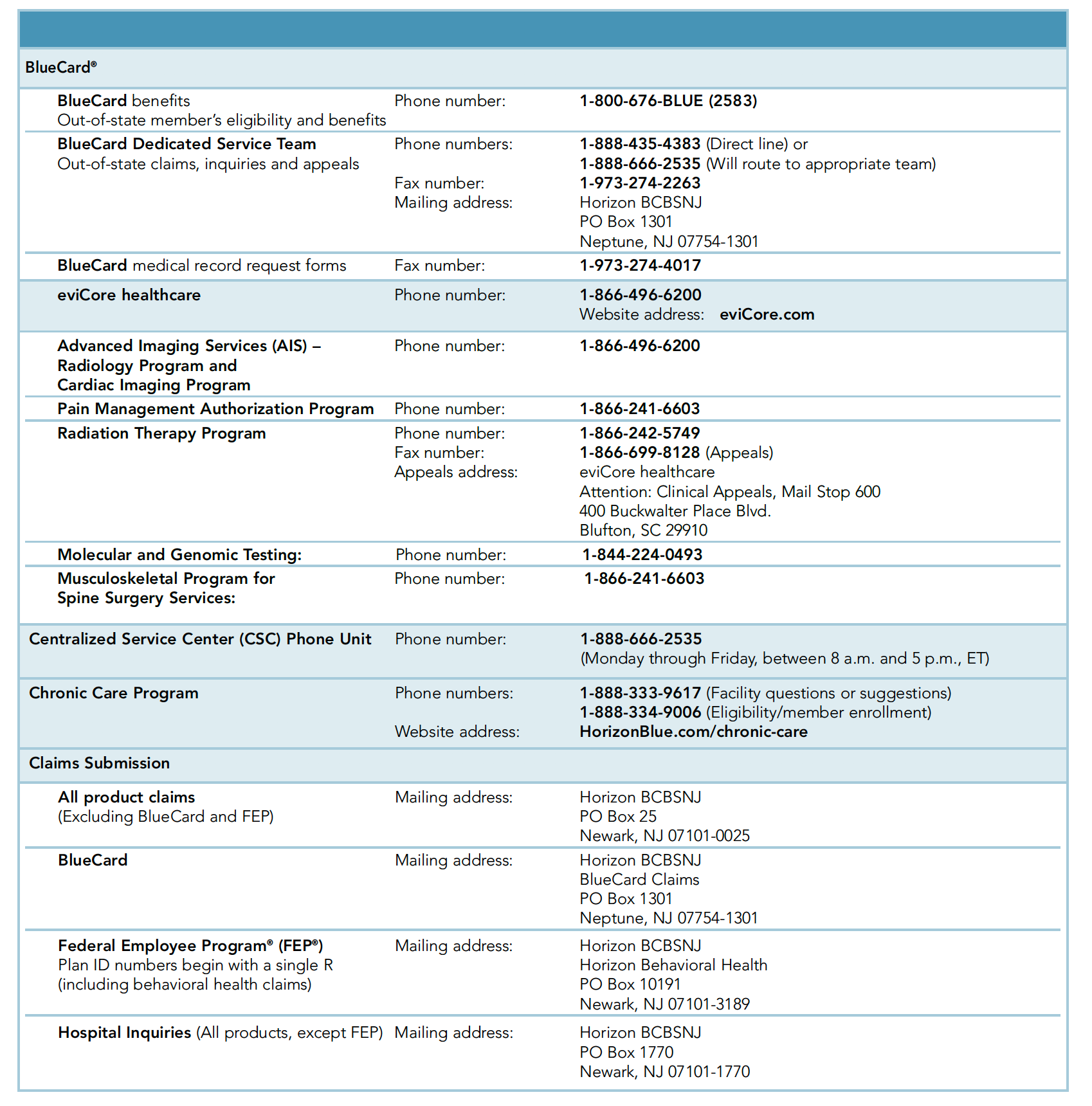
Service Horizon Blue Cross Blue Shield Of New Jersey
Weve taken steps to lower costs and provide our members easier access to care related to COVID-19.
Does blue cross fep cover covid antibody test. Yes antibody tests for COVID-19 testing are covered at 100 with no member cost sharing as required by the Families First ActCARES Act. Labcorp will bill the cost of the COVID-19 antibody test directly to your health plan if you are insured or if you are uninsured Labcorp will bill the appropriate government program. To be covered by CareFirst the test should.
A nurse case manager with Blue Cross Blue Shield of Rhode Island found that listening without judgment to one patients concerns made all the difference. However antibody testing does NOT indicate if an individual has an active COVID-19 infection. 31 were waiving the cost share for covered services for the treatment of those with a positive COVID-19 diagnosis.
However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary. It does not include testing for people without symptoms and no suspected exposure. The COVID-19 test is 0 for all members and through Aug.
Please talk to a doctor first to be certain you need a COVID-19 test. To be covered by your BCBSRI health plan your COVID-19 test must be medically necessary and ordered by a healthcare provider. Thats a big step toward stopping the spread of the virus.
Information about serological test performance characteristics are displayed in this Independent Evaluation of SARS-CoV-2 Antibody Test Performance. Blue Shield and Blue Shield Promise cover most diagnostic tests for individuals at no out-of-pocket cost to you. Testing and Treatment Coverage.
No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19. This includes testing for people who have been exposed or may have been exposed to someone with COVID-19. COVID-19 testing is available at no cost.
People booking a PCR test for COVID-19 will also be given the option to take part in antibody testing. Exclusions to this coverage include testing for the following. Be on the EUA list.
Tests with FDA Emergency Use Authorization have varying degrees of accuracy. See below for those not covered This means you do not need to pay out-of-pocket costs copay coinsurance or deductible for tests that are provided or ordered by a healthcare provider. That is why our Florida Blue Center teams are here to provide support for you and your patients.
Lab tests to diagnose COVID-19 are covered at no cost. No prior authorizations for diagnostic tests and covered services FEP will waive prior authorizations for diagnostic tests and for covered services that are medically necessary and consistent with CDC guidance if diagnosed with COVID-19. This includes screenings andor tests that take place at in-person office visits drive-through sites virtual on-line visits and telephone calls.
Thats why during this time FEP is making some benefit changes to ensure you have access to the right care at the right time. No prior authorizations for diagnostic tests and covered services. The FDA has approved several vaccines for emergency use authorization.
That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. Call us at 877-352-5830 with questions about COVID-19. All Anthem plans will cover medically necessary screening and testing for COVID-19 and will waive all cost shares co-pays coinsurance and deductibles.
If you charge the member a cost share at the time of service you may need to reimburse the member when you receive your voucher. Be ordered by a physician or other authorized provider. Part B covers certain doctors services outpatient care medical supplies and preventive services.
Covers a COVID-19 antibody or serology test. The cost of the test is 4213 and is based on rates established by the Centers for Medicare Medicaid Services CMS. Antibody testing is not currently recommended to assess for immunity to COVID-19 following vaccination.
No cost share for diagnostic tests or treatment. To ensure you have access to the right care at the right time FEP is waiving cost shares and prior authorization to support members care for COVID-19. Yes Blue Cross Blue Shield members will not have to pay for COVID-19 diagnostic tests that are performed by a licensed or authorized health care provider through October 18 2021.
In accordance with the Families First Coronavirus Response Act CareFirst is covering the antibody test for SARs-CoV-2. Use the doctors labs and facilities in your BCBSIL health plans provider network for. No early medication refill limits.
Through May 31 all BCBS companies including the BCBS Federal Employee Program FEPare. Tests to diagnose COVID-19. Coronavirus disease 2019 COVID-19 antibody test.
Find a COVID-19 testing location near you by using this tool. We suggest you bill Blue Cross or BCN first for COVID -19-related services and wait for the voucher remittance advice to determine member cost share liability. With a BCBSIL health plan you have access to care for COVID-19 related health issues.
We have transitioned our walk-in Florida Blue Centers to virtual support and services and our locally based nurses community specialists and service specialists are just a phone call away. When are COVID-19 tests covered. Have a high likelihood of impacting clinical decision making.
Waiving cost-sharing for COVID-19 testing and treatment. No cost share for COVID-19 vaccines. More than 140 million Americans have received a dose of the COVID-19 vaccine.
Blue Cross and Blue Shield of Illinois BCBSIL is closely monitoring activity around the Novel Coronavirus 2019 COVID-19. An antibody test does not detect the presence of the SARS-CoV-2 virus to diagnose COVID-19. BCBSTX is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order.
Your Blue Cross and Blue Shield of Illinois BCBSIL health plan gives you access to the care you need during the COVID-19 pandemic. For testing performed out of network CareFirst or the plan sponsor will pay 100 up to charge. Are antibody tests used to diagnose COVID-19.
All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs. You can still get an antibody test if youve had the COVID-19 vaccine. But some are still hesitant to get the shot.
CareFirst and plan sponsors will cover the full cost of in-network deductibles copays and coinsurance for FDA-authorized and medically necessary antibody testing when ordered by a doctor nurse practitioner or other authorized provider.
/coronavirus-antibody-test-uses-4844950-no-logo-8598c6cbd7b140a1b3ec50071f2e69f6.gif)
Coronavirus Antibody Test How It Works Accuracy Where To Get One

Covid 19 Info For Clinical Partners

Blue Cross Coverage Of Covid 19 Testing What To Know Mibluesperspectives

Covid 19 Coronavirus Resource Center Benefit Changes Blue Cross And Blue Shield S Federal Employee Program

Coronavirus Updates Blue Cross Of Idaho

Covid 19 Coronavirus Resource Center Benefit Changes Blue Cross And Blue Shield S Federal Employee Program

Information Regarding Coronavirus Covid 19 Highmark Bcbswny
Coronavirus Your Health Care Premera Blue Cross

Bcbs Covid 19 Info Benefits Testing And More Blue Cross And Blue Shield S Federal Employee Program
Bluecross Blueshield Of South Carolina And Bluechoice Healthplan Of South Carolina Inc Group Eligibility Guidelines Related To Covid 19 Pandemic Bluechoice Healthplan Of South Carolina

Your Frequently Asked Questions About Covid 19 Coronavirus

Bcbs Covid 19 Info Benefits Testing And More Blue Cross And Blue Shield S Federal Employee Program

Testing For Covid 19 Faqs Blue Shield Of Ca

Covid 19 Info For Clinical Partners


Posting Komentar untuk "Does Blue Cross Fep Cover Covid Antibody Test"