Does Insurance Cover Rapid Covid Test Cvs
Because serological tests for COVID-19 meet the definition of in vitro diagnostic tests for the detection of SARS-CoV-2 or the diagnosis of COVID-19 serological tests are covered by TRICARE if they are determined to be medically necessary To be medically necessary means it is appropriate reasonable and adequate for your condition. If your insurance does not cover the test the cost is 135.

Covid Testing Same Day Rapid Results 936 Willow Road Northbrook Il Minuteclinic
The exact cost you incur may vary but out-of-pocket costs for COVID-19 tests generally hover between 100 and 150.

Does insurance cover rapid covid test cvs. Covers a test to see if you have coronavirus officially called coronavirus disease 2019 or COVID-19. On top of that there may also be costs associated with the office or clinic visit. Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a licensed healthcare provider.
If you have health insurance you must bring your card with you to the test site. One couple paid 139 each for a test before traveling to Hawaii and told Noozhawk their Medicare insurance wouldnt pay for the CVS tests. Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you.
Tests must be provided or ordered by a healthcare provider licensed or authorized to provide or order COVID-19 tests. Large-scale rapid COVID-19 test sites Beginning in March 2020 CVS Health took a leadership role in addressing the need for increased and convenient access to COVID-19 testing across the US. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings.
According to its website UnitedHealthcare members will have 0 cost-share copay coinsurance or deductible for COVID-19 testing-related visits through Jan. If you have health insurance you must bring your card with you to the test site. While vital testing is costly or can be.
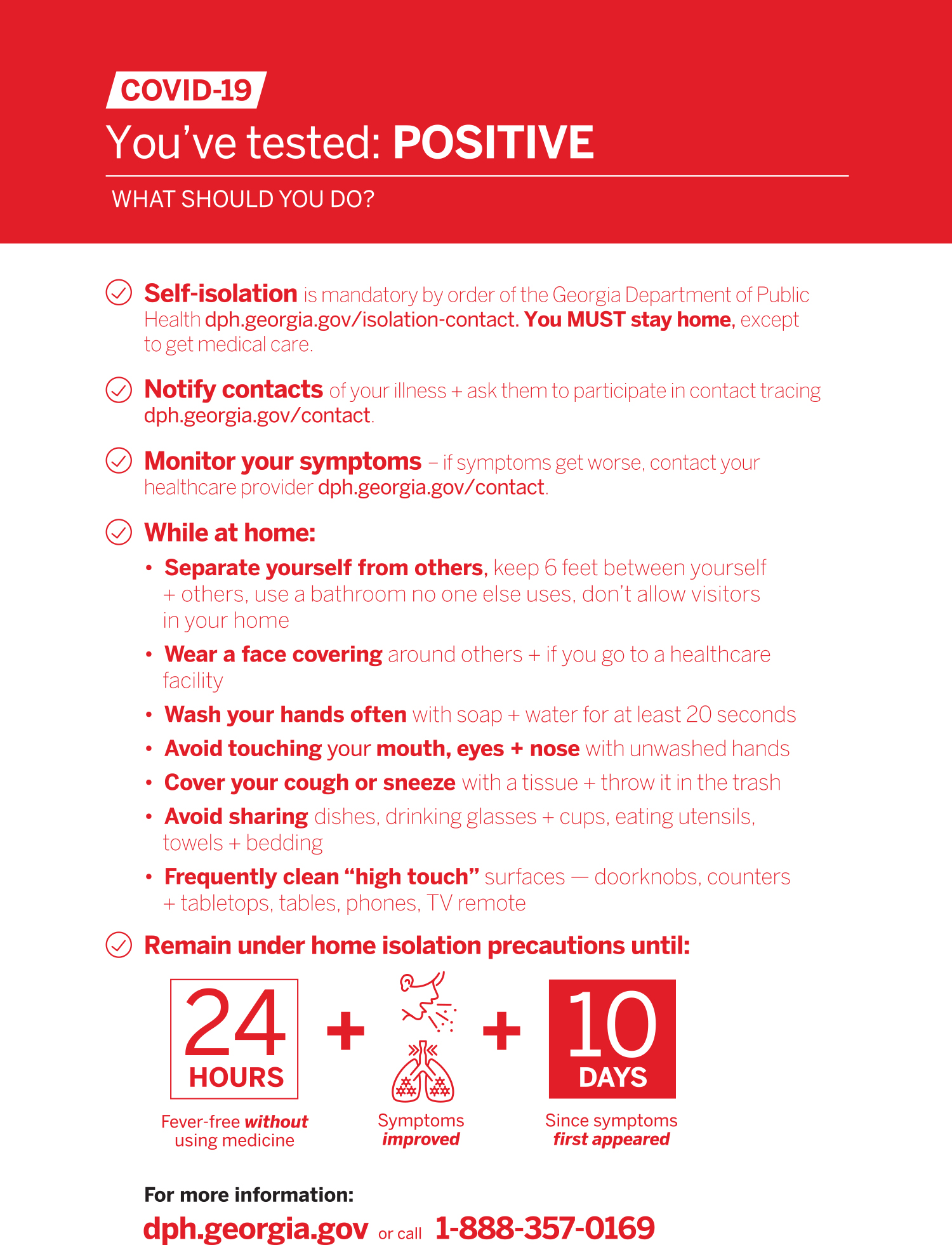
However it remains uncertain whether individuals with antibodies are protected against reinfection with COVID-19. For patients who test negative for COVID-19 through a rapid test and come into the clinic the clinic visit should be considered part of your test by. Tufts Medical Center conducts tests in Boston with results in 48-72 hours.
Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19 serological antibody testing with no cost-sharing. When are COVID-19 tests not. 1-800-557-6059 TTY 711 247.
CVS will be offering rapid tests for COVID-19 Justin SullivanGetty Images. No rapid covid tests have full FDA approval. 2 Walgreens website listed its additional charge as 29 and CVS listed a 39 extra charge for the PCR test.
The rapid test at Walgreens is listed at 49 total. For patients who test negative for COVID-19 through a rapid test and come into the clinic the clinic visit should be considered part of your test by your health. Patients with insurance should not have any out-of-pocket costs for a covered COVID-19 test but you should check with your health plan to confirm before scheduling a test.
Medicare Advantage Plans are allowed to waive cost-sharing for COVID-19 lab tests. CVS Health will offer rapid-result COVID-19 testing at almost 1000 of their pharmacies by the end of 2020 according a recent news release. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
Two rapid molecular options made by Lucira Health and Cue Health also have emergency use authorization EUA. What does Medicare cover. Medicare pays for all diagnostic COVID-19 tests.
CVS Health has been increasing access to testing options since the start of the pandemic and has completed more than 15 million COVID-19 tests to date across more than 4800 testing sites at select CVS Pharmacy locations with nearly 1000 of those locations providing. Standard PCR tests sent to a lab. As announced by CMS starting January 1 2021 Medicare will make an additional 25 add-on payment to laboratories for a COVID-19 diagnostic test run on high throughput technology if the laboratory.
Medicare covers lab tests for COVID-19 with no out-of-pocket costs. Walgreens CVS and Rite Aid all have COVID-19 tests available for travel. Medicare covers all medically necessary hospitalizations.
Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services. DM Covid-19 Test conducts curbside tests at their Columbia office. Food and Drug Administration FDA approved COVID-19 home tests that you buy at a pharmacy or store without a prescription or order from a licensed health care professional are not covered by your planMost health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional.
Its 219 for same-day results or 299 for results in one hour. Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing using tests approved by. As of Wednesday Dec.
The OTC testing options are not covered by insurance and are not meant to test the efficacy of COVID-19 vaccination. First youre doing the smart thing by getting tested before traveling. Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit.
Medicare reimburses up to 100 for the COVID test. A completes the test in two calendar days or less and b completes the majority of their COVID-19 diagnostic tests that use high throughput technology in two calendar days or less for all of. Once a COVID-19 vaccine becomes available it will be covered.
We rapidly stood up a pilot drive-thru rapid COVID-19 test site in the parking lot of. A note about antibody tests Serology tests detect the presence of antibodies produced after exposure to the virus. Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered.
Patients with insurance should not have any out-of-pocket costs for a covered COVID-19 test but you should check with your health plan to confirm before scheduling a test. Therefore the CDC does not recommend serology tests to determine when it is safe for a person to return to work. And second youre in luck.
Blue Shield and Blue Shield Promise cover these diagnostic tests.

At Home Covid 19 Test Pixel By Lapcorp Cvs Pharmacy

Cvs Health Expands Covid 19 Testing Services Adds 1 000 Rapid Result Test Sites Healthcare Finance News
Cvs Pharmacy Frequently Asked Questions

Masaschusetts Among Places Where Cvs Will Add Rapid Covid 19 Testing Boston Business Journal

List Of Retailers Offering Coronavirus Testing

Quidel Corporation Quidel To Bring Quickvue At Home Otc Covid 19 Tests To Cvs Pharmacy

Binaxnow Covid 19 Antigen Self Test

Cvs Health Announces Availability Of Covid 19 Antibody Testing In All Minuteclinic Locations In Texas Cvs Health

Cvs Health To Offer Covid 19 Antibody Testing At All Minuteclinic Locations Wpri Com

At Home Covid 19 Test Pixel By Lapcorp Cvs Pharmacy

Cvs Health Announces Availability Of Covid 19 Antibody Testing At Minuteclinic Locations Across The Country Cvs Health
Local Covid 19 Testing Available Throughout New Hanover County

Cvs Health Announces Availability Of Covid 19 Antibody Testing In All Minuteclinic Locations In Massachusetts Cvs Health

Binaxnow Covid 19 Antigen Self Test

Over The Counter Covid 19 Testing Now Available At Cvs Pharmacy Ellume

At Home Covid 19 Test Pixel By Lapcorp Cvs Pharmacy

Posting Komentar untuk "Does Insurance Cover Rapid Covid Test Cvs"