Will Medicaid Cover Covid Testing
More Information To learn more about COVID-19 Coronavirus Georgia Medicaid members and providers should visit the Centers for Disease Control and Prevention and Georgia Department of Public Health websites. Service use among Medicaid CHIP beneficiaries age 18 and under during COVID-19.
Faqs On Medicare Coverage And Costs Related To Covid 19 Testing And Treatment Kff
When tests are available for you in your state Medicare covers and you pay nothing for.
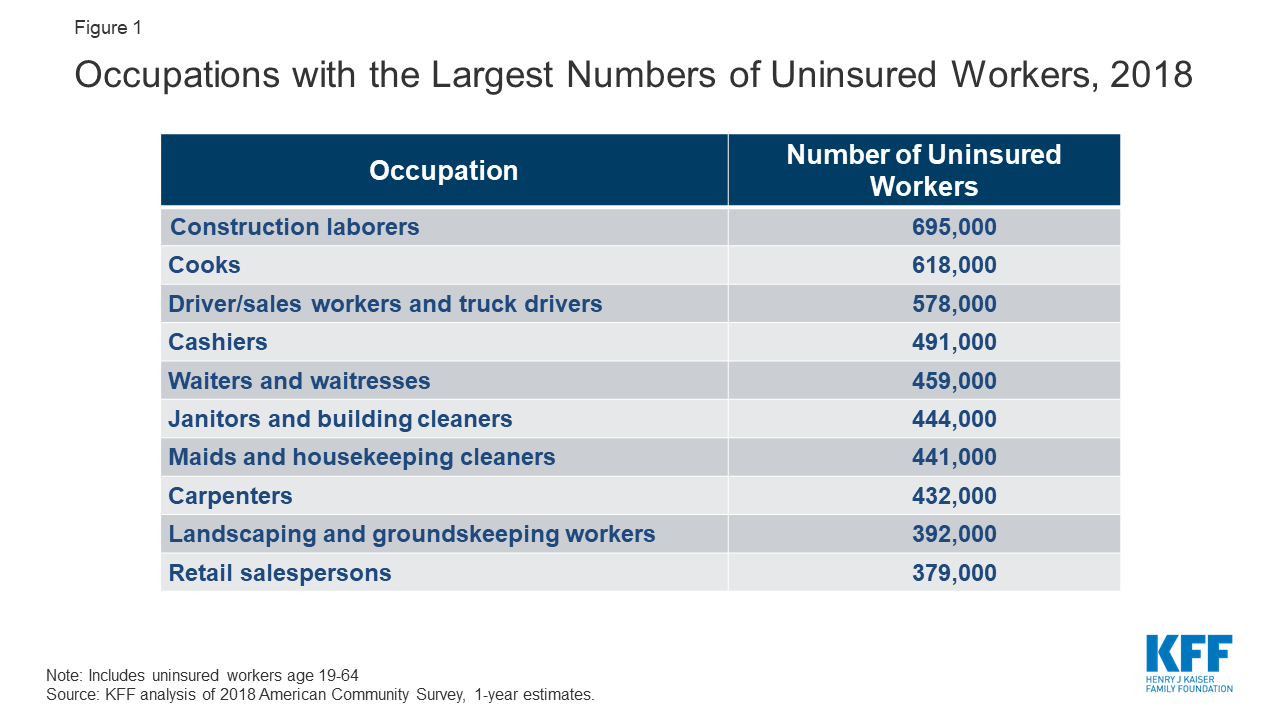
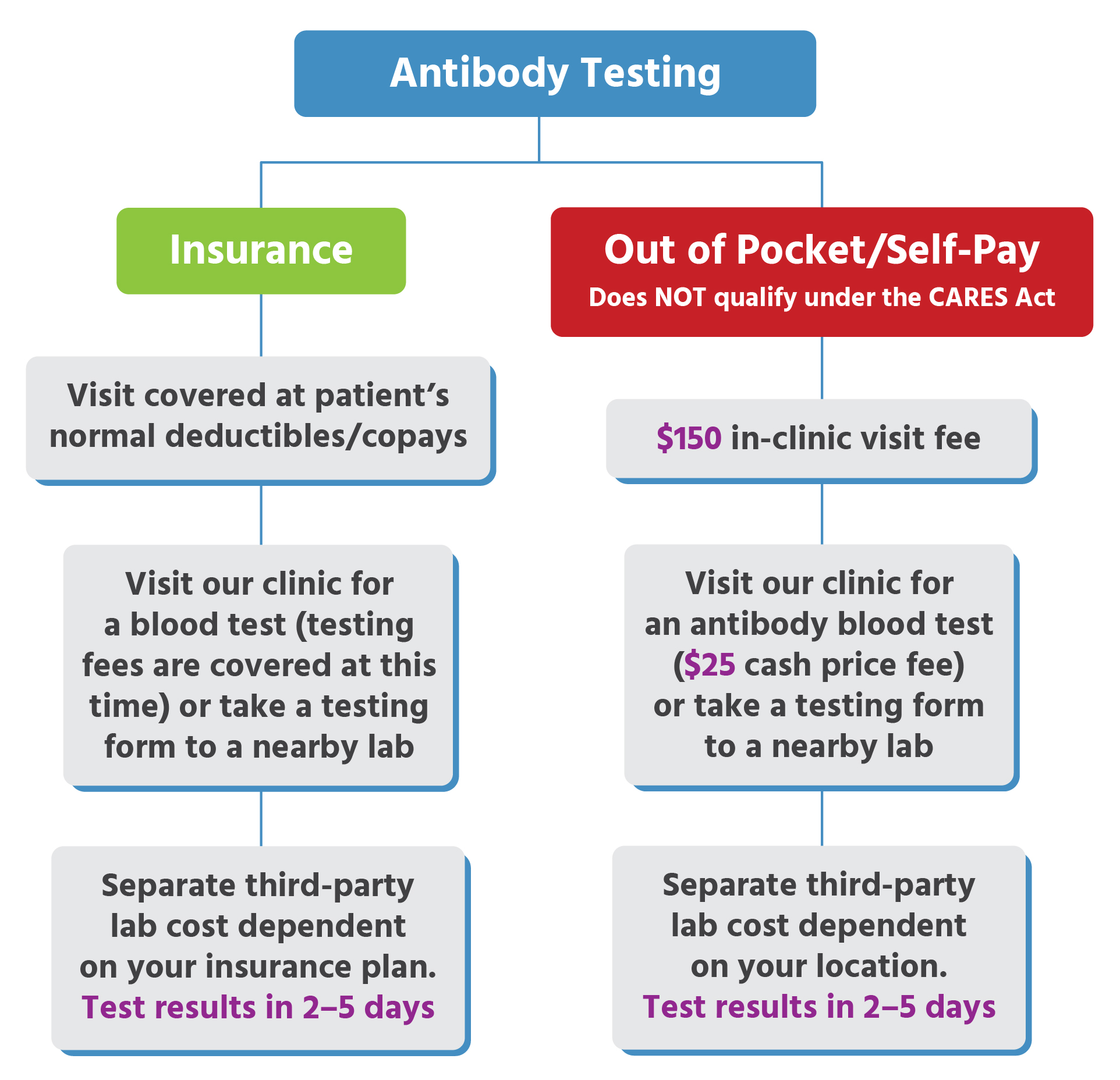
Will medicaid cover covid testing. Medicaid must also cover testing and treatment for COVID-19. Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19 serological antibody testing with no cost-sharing. SCDHHS has also made a number of temporary policy changes to ensure ongoing access to care during the COVID-19 pandemic including creating additional ways to submit documents electronically to the.
The fees below are. Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. Your healthcare provider will work with local public health officials to determine if you should be tested for COVID-19.
We will cover medically necessary COVID-19 diagnostic testing medical screening services andor treatment at no charge to you when such services are ordered andor referred by a. New York State NYS Medicaid Billing Guidance for COVID-19 Testing Specimen Collection and Monoclonal Antibody Infusions. The services in this guidance document are currently reimbursable by NYS Medicaid fee-for-service FFS and Medicaid Managed Care MMC Plans.
COVID-19 testing is a covered benefit for current Healthy Connections Medicaid members including those enrolled in Family Planning so they do not need to apply for the new program. The Centers for Medicare Medicaid Services CMS released six sets of general Frequently Asked Questions FAQs to aid state Medicaid and Childrens Health Insurance Program CHIP agencies in their response to the coronavirus disease 2019 COVID-19 pandemic. Preliminary Medicaid CHIP Data Snapshot Services through May 31 2020 PDF 112 MB Other Resources Coverage and Reimbursement of COVID-19 Vaccines Vaccine Administration and Cost-Sharing under Medicaid the Childrens Health Insurance Program and Basic Health Program Toolkit.
For State Medicaid and Childrens Health Insurance Program CHIP Agencies. The Medicare programmes are overseen by the Centers for Medicare and Medicaid Services CMS an. In an effort to implement the Biden-Harris Administrations Build Back Better Agenda in Americas classrooms and communities CMS is reinforcing that Medicaid will cover diagnostic and screening testing for COVID-19 when that testing is consistent with Centers for Disease Control and Prevention CDC recommendations.
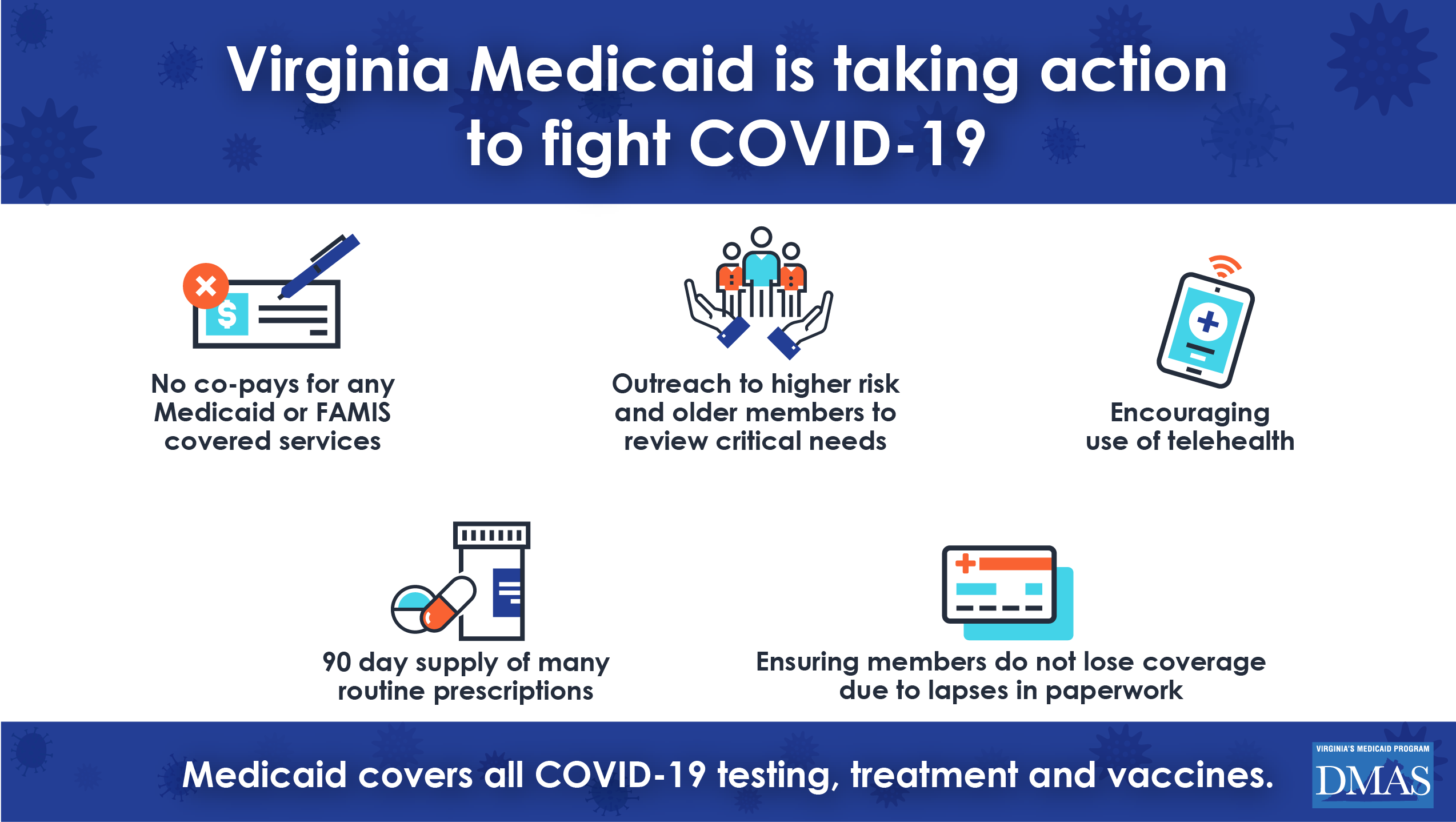
COVID-19 Testing in Schools. UPDATES are highlighted in YELLOW. Thanks to a provision in the American Rescue Plan Act state Medicaid programs are required to cover COVID-19 vaccines and any administration fee that may apply.
The COVID-19 test will be covered by Medicaid Medicare and private insurance plans Vice President Mike Pence said Wednesday. For information on the testing and treatment of the uninsured for COVID-19 see the resources section of this page. Does Medicare cover covid-19 testing.
No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid. Medicaid Coverage of Coronavirus Testing Alert Rapid Lab Test and Antibody Test Provider Alert Additional Guidance on Antibody Testing Alert Exceed Service LimitsExpand Coverage. What does Medicaid cover.
In an effort to implement the Biden-Harris Administrations Build Back Better Agenda in Americas classrooms and communities CMS is reinforcing that Medicaid will cover diagnostic and screening testing for COVID-19 when that testing is consistent with Centers for Disease Control and Prevention CDC. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. Find a free COVID-19 vaccine near you.
Medicare provides coverage for millions when it comes to covid-19 and in most cases beneficiaries will not pay a single dollar out of pocket. What are the differences. Refer to the NYS Medicaid Billing Guidance for COVID-19 testing and Specimen collection for information on COVID-19 diagnostic tests with at home sample collection.
Does Medicare cover covid-19 testing. Does Medicaid cover the COVID-19 vaccine. Medicare covers these tests at different locations including some parking lot test sites.
HHS has already denominated a. During the Public Health Emergency PHE and for more than a year after it ends Medicaid is required to cover COVID-19 testing vaccinations and treatment for most enrollees and it may not charge cost sharing for these services. NYS Medicaid FFS will not cover tests that are over-the counter or purchased for at home use.
Coverage and Benefits Related to COVID-19 Medicaid and CHIP Medicaid and the Childrens Health Insurance Program CHIP provide health coverage to millions of Americans including eligible low-income adults children pregnant women elderly adults and people with disabilities. Exceed service limits to maintain the health and safety of recipients diagnosed with COVID-19 or when it is necessary to maintain a recipient safely in their home inpatient home health etc. Medicaid and CHIP are funded jointly by states and the.
Tests to diagnose or aid the diagnosis of COVID-19. Medicaid and CHIP will cover COVID-19 testing for Medicaid and CHIP clients. Covers a COVID-19 antibody or serology test.
Coronavirus disease 2019 COVID-19 antibody test. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services.
Medicaid and CHIP will cover COVID-19 testing for Medicaid or CHIP clients. COVID-19 Testing in Schools. Governor Kemp and the Georgia Health Care Association issued a joint statement on March 16 2020 with new guidance from the Centers for Medicare and Medicaid Services.
Utah has announced that the state Medicaid program will cover the cost of COVID-19 testing for uninsured residents starting June 1 2020. No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid.
What Issues Will Uninsured People Face With Testing And Treatment For Covid 19 Kff

Medicaid And Chip Flexibility Can Help Safeguard Americans During The Covid 19 Crisis Urban Institute

Covid 19 Resources For Health Care Access In Washington State Northwest Health Law Advocates
Urgent Care For Kids Antibody Testing Locations

Home Tests Could Help In The Fight Against The Coronavirus So Where Are They The Washington Post
Covid 19 Test Sites Washington County Of Utah
![]()
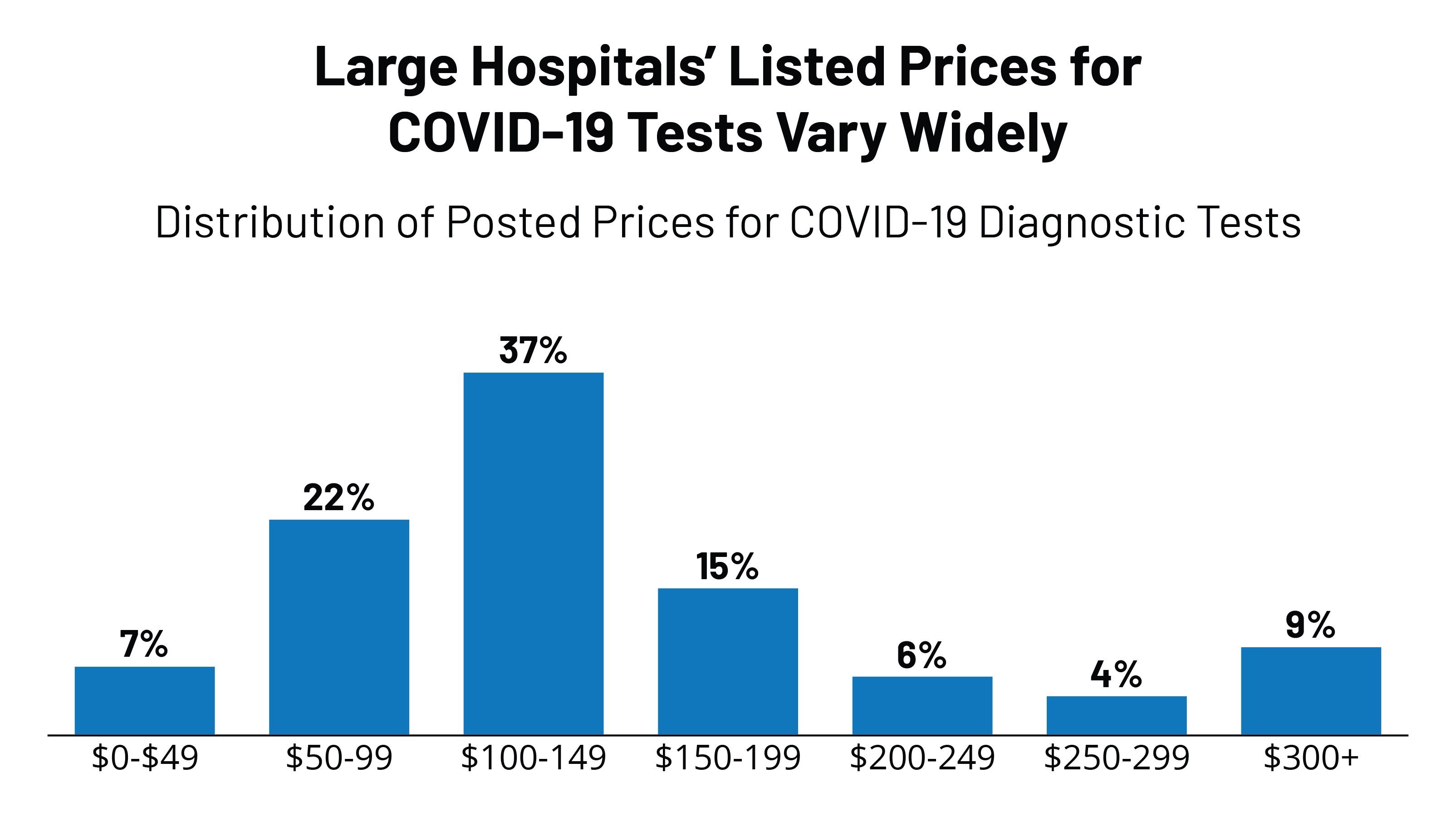
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr
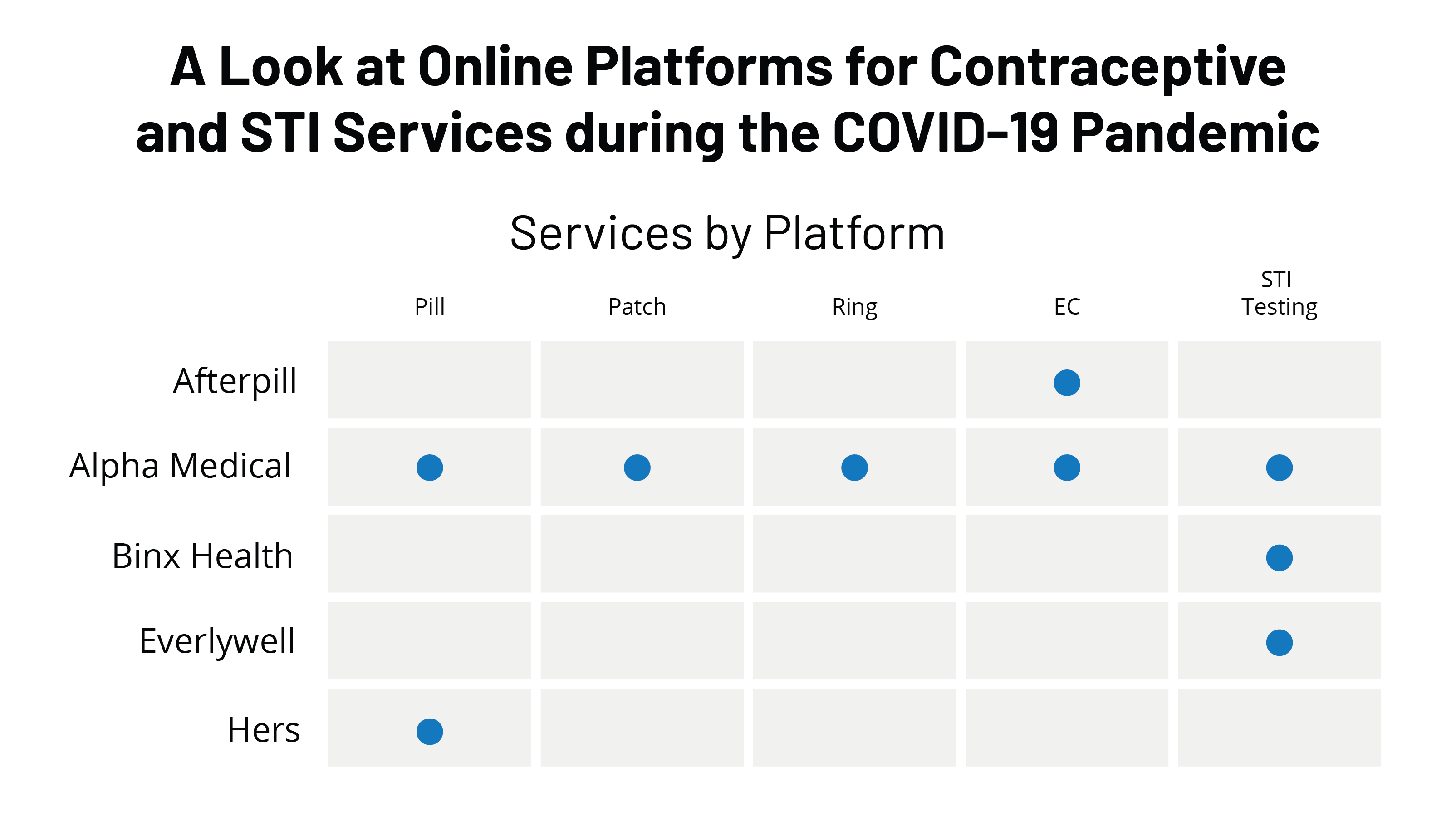
A Look At Online Platforms For Contraceptive And Sti Services During The Covid 19 Pandemic Kff
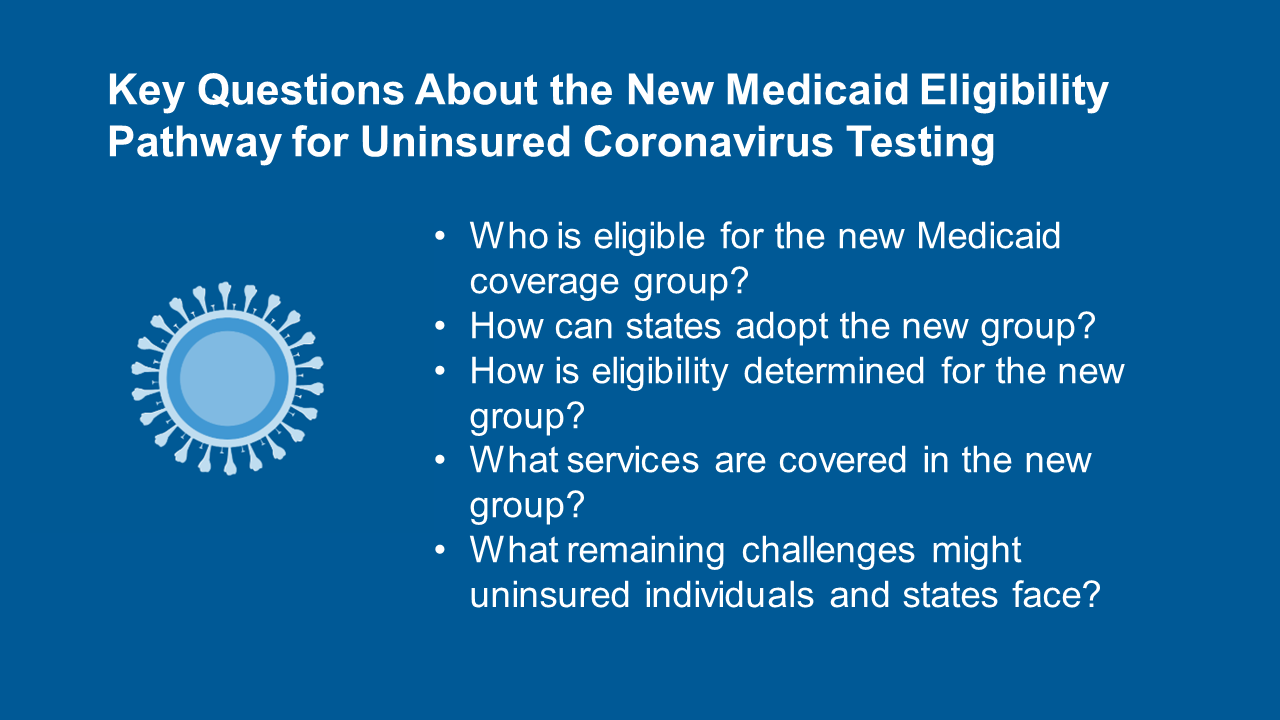
Key Questions About The New Medicaid Eligibility Pathway For Uninsured Coronavirus Testing Kff
Covid 19 Testing Is Available For Free At A Location Near You Chinese American Planning Council

Covid 19 Testing Sites West Side United

We Can Solve The Coronavirus Test Mess Now If We Want To The New Yorker

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

The Laws Governing Covid 19 Test Payment And How To Improve Them

Lugares Donde Puedes Hacerte La Prueba De Covid 19

Posting Komentar untuk "Will Medicaid Cover Covid Testing"