Does Insurance Cover Covid Testing Cigna
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. Cigna increased the weighting factor of the assigned Medicare DRG by 20 for members hospitalized with a COVID-19 diagnosis and discharged during the COVID-19 Public Health Emergency PHE period.
Iso International Student Insurance
CI customers will have access to coronavirus COVID-19 testing as prescribed.

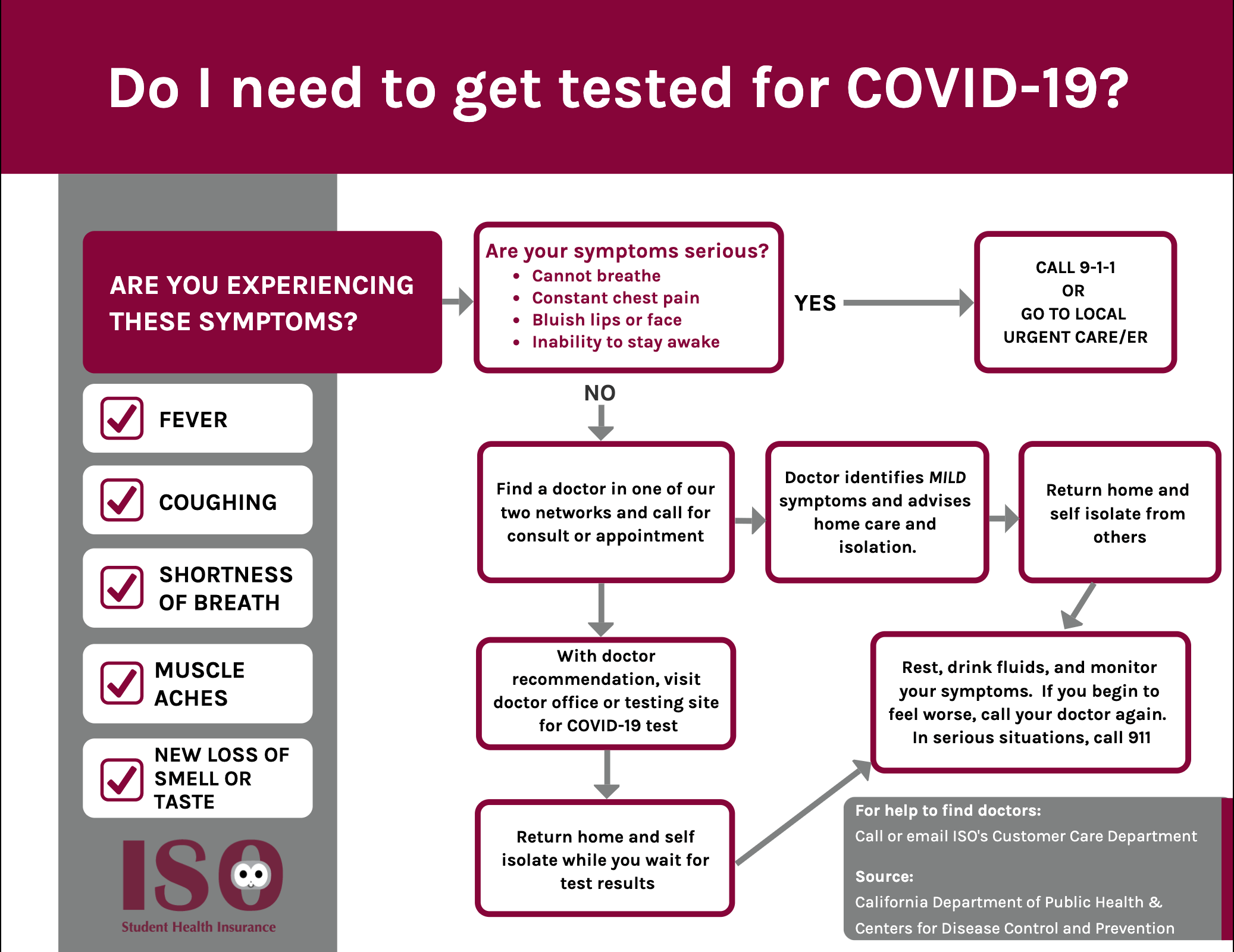
Does insurance cover covid testing cigna. November 6 2020. Yes most likely you can still get health insurance if you have been diagnosed with COVID-19 but the insurance company might exclude Coronavirus from your coverage. Complete an online screening.
We only cover the cost of PCR testing when requested by a medical professional. Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. Dozens of insurers including Aetna Cigna and Humana.
This will continue as long as state and federal mandates for the coverage of testing without out-of-pocket costs apply. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests as required by the CARES Act. We do not cover the cost of antibody testing. Cigna stated that it is unable to share specific details about this individuals sic claim because of health privacy laws.
Enhanced coverage for COVID-19 diagnostic testing office exams telehealth screenings and virtual care applies to customers in the United States who are covered under Cignas employerunion sponsored insured group health plans insured plans for globally mobile individuals Medicare Advantage Medicaid and the Individual and Family insurance plans. They may also cover testing for recovered COVID-19 patients who want to donate antibody-rich plasma for treatment of others or for children with a rare coronavirus-related complication. If you have insurance in-network with Carbon Health your insurance plan must cover diagnostic COVID-19 testing without patient cost sharing whether you are asymptomatic or symptomatic andor do not have a confirmed exposure.
For Medi-Cal members all tests are fully covered at no cost to members. Testing is expected to expand shortly as more commercial testing becomes available at a designated lab approved by the United States Food Drug Administration. The CARES Act also requires insurers to cover the testing without any prior authorization requirements or imposing cost-sharing on patients.
A complaint was filed today against Cigna Health and Life Insurance by Murphy Medical Associates regarding the provision of COVID-19 testing in the state of Connecticut. Americas Health Insurance Plans is calling on more government support to cover the cost of COVID-19 tests which it says could be between 6 billion and. Treatment co-pays and co-insurance.
This is because insurance companies will consider COVID-19 as a pre-existing condition. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your family gets COVID-19 you wont have to. Anthem does not specify a limit on the number of COVID-19 tests it will cover.
Medicaid will cover the full cost of COVID-19 testing for the uninsured as directed by the CARES Act. Cigna will not reimburse providers for the cost of the vaccine itself. Diagnostic tests are covered for individuals with symptoms of a COVID-19 infection or who had exposure to someone with a suspected or confirmed COVID-19 infection as well as for individuals before an elective hospital admission or procedure.
Self-initiated at-home specimen collection kits that are FDA-approved such as the Pixel by LabCorp testing kit will be covered by Cigna cost share waived. You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share. REQUEST A HOME TESTING KIT This COVID-19 treatment policy applies to customers in the United States who are covered under Cignas employer-union-sponsored insured group health plans insured plans for US-based.
Cigna has committed to covering the medical test similar to a preventive benefit for fully-insured plans thereby waiving co-pays coinsurance or deductibles for customers. For further details on testing and our policy please refer to Will you pay for the cost of COVID 19 testing below. Diagnostic testing generally means a symptomatic or asymptomatic individual seeks and receives a COVID-19 test from a licensed or authorized health care provider or when a licensed or authorized health care provider refers an individual for a COVID-19 diagnostic test ie when an individual customer wants to be tested for any reason and seeks out a test on their own.
According to Ellison a Cigna representative told him the insurance firm is among the carriers that agreed to waive all out-of-pocket expenses for COVID-19 testing. The following information is for COVID-19 testing only and does not apply to a regular visit to a Carbon Health clinic or any non-coronavirus related visits. Out-of-pocket testing costs for COVID-19 individual diagnostic tests will be waived during the federal public health emergency.
Cigna Health According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing. Additional FDA EUA approved vaccines will be covered consistent with this guidance. Provide your Cigna insurance information.
For additional information about our coverage of the COVID-19 vaccine please review our COVID-19 Vaccine coverage policy.

Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

What To Know About Coronavirus Your Insurance Utah Insurance Department

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Payers Begin To Pay Individual Small Group Rebates Amid Covid 19
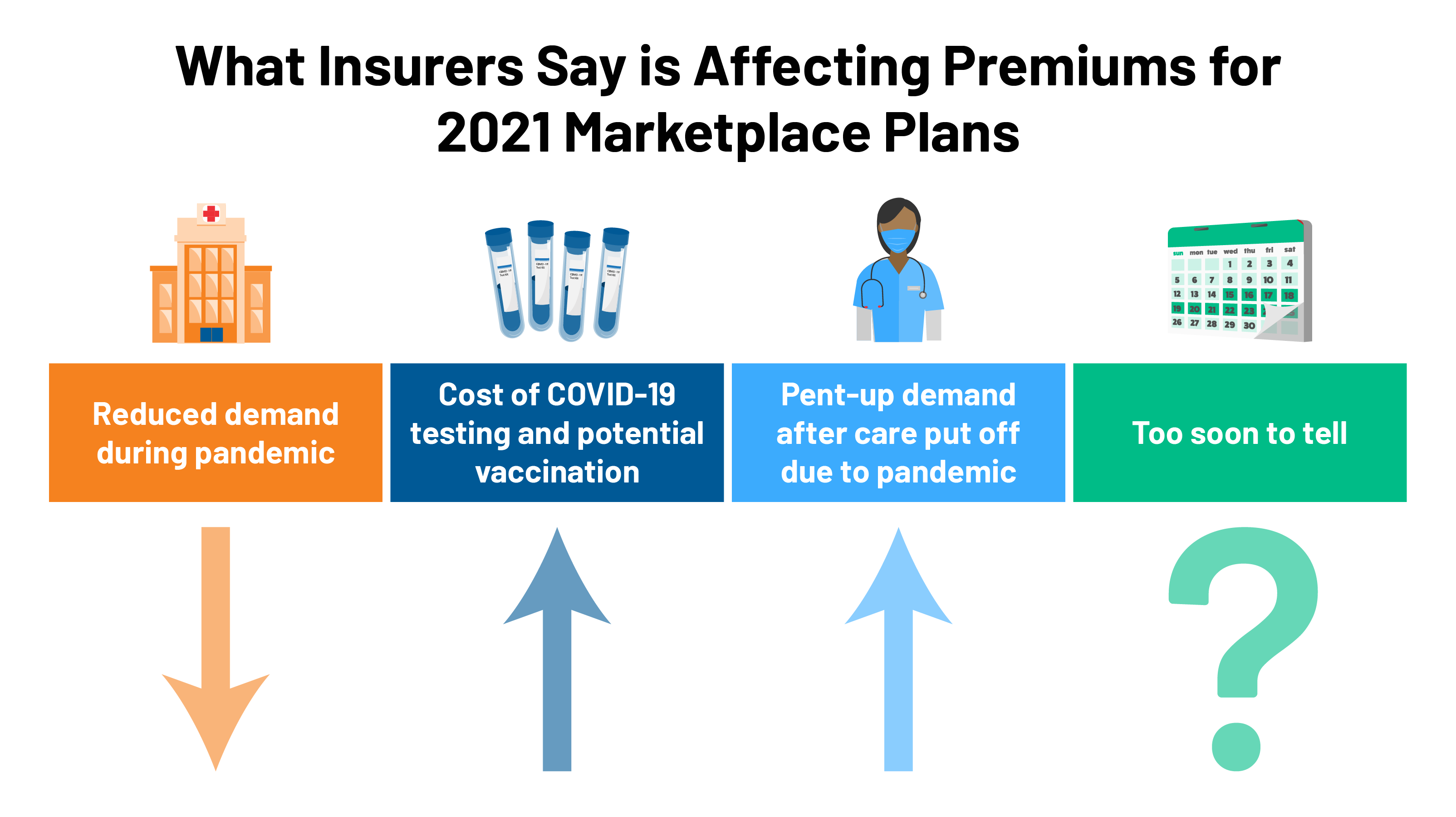
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Cigna And Humana Waive Coronavirus Treatment Costs

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna Raises Financial Forecast For 2021 Despite The Ongoing Covid 19 Pandemic Healthcare Finance News

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Posting Komentar untuk "Does Insurance Cover Covid Testing Cigna"